Guidance to Reduce Risk of COVID-19 When Handling Wildlife
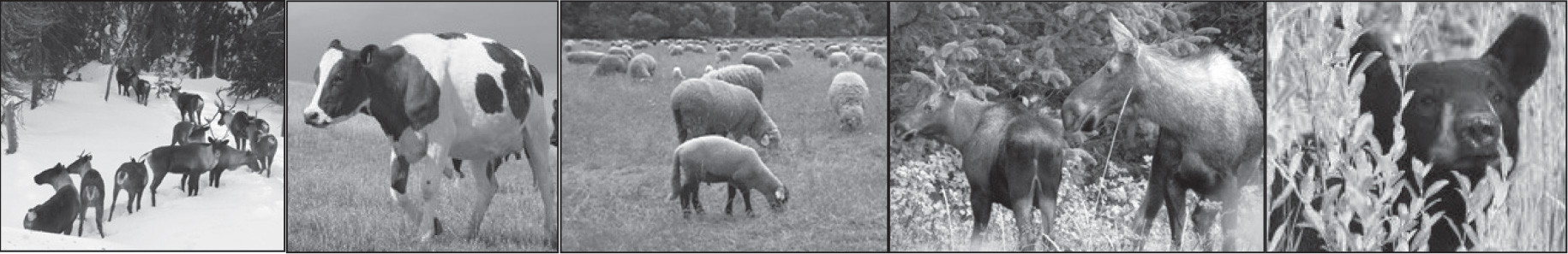
Canada and the United States have recently reported the presence of SARS-CoV-2, the virus that causes COVID-19, in wild white-tailed deer, providing the first evidence that the virus can circulate in wild animal populations. Studies have revealed that the virus has spread from humans to deer on multiple occasions, with subsequent spread from deer to deer. To date, there has been no known transmission of SARS-CoV-2 from white-tailed deer to humans. There is potential risk that those in contact with infected deer or carcasses could be exposed to the virus. Up-to-date vaccination remains one of the most effective ways to help protect yourself, your family, and your community against COVID-19.
Currently there have been no known cases of SARS-CoV-2 in game species in Newfoundland and Labrador and the susceptibility of other animals such as moose, caribou and other game species is unknown in Canada. Bird species are not susceptible to COVID-19. Efforts to monitor wildlife diseases, including SARS-CoV-2, are ongoing throughout Canada.
Until more is known, to help protect yourself and reduce your risk while hunting or trapping, it is recommended that you wear a well-fitting mask and practice good hand hygiene. Additional recommendations for handling and dressing the carcass are available on the Government of Canada’s Animals and COVID-19 webpage and on the Canadian Wildlife Health Cooperative’s COVID-19 webpage.
Government of Canada – Animals and COVID-19: www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks/animals-covid-19.html
Canadian Wildlife Health Cooperative – COVID-19: www.cwhc-rcsf.ca/covid-19.php
Avian Influenza
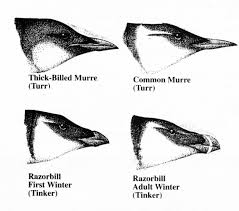
Avian influenza, or “bird flu”, occurs in many strains and is a contagious viral infection that normally affects a variety of wild bird species, food producing birds, and pet birds. The virus is classified into two categories, low pathogenicity and high pathogenicity, depending on the severity of the illness in birds.
Influenza viruses are very adaptable, and occasionally there are strains that adapt to infect other animals. Recently there is a high pathogenicity strain in birds (H5N1), that can also rarely infect mammals including humans.
Although H5N1 spreads easily in birds and usually causes severe symptoms in bird species, it is rare for transmission to humans to occur and symptoms in humans are usually more subdued. Infected people may not develop any symptoms at all. However, if symptoms do develop, illness can range from mild to very severe, rarely including death. Human symptoms include cough, shortness of breath, achy muscles, conjunctivitis, headache, and other flu-like symptoms. If you are concerned you have been exposed to Avian Influenza, contact your physician for advice.
Human infection is most common through close contact with infected birds or time spent in heavily contaminated environments (feather dust or bodily secretions). With the potential risk for human infection, it is highly recommended that people handling birds that may be infected with avian influenza wear protective equipment such as face masks, goggles, gloves, and boots. If you come across multiple sick or dead birds in close proximity, do not handle the birds and instead call your local regional services office.
There is no evidence of Avian Influenza being transmitted through meat or eggs that are properly cooked.
Information regarding avian influenza from the Government of Canada can be found here.
Giardiasis
Also known as Beaver Fever is caused by a parasite: Giardia lamblia
Contracted by mouth, usually by drinking contaminated water. This parasite is passed on via feces of infected animals such as human and beaver. However, it may also be contracted by putting something in your mouth that has come in contact with the parasite. Symptoms include diarrhea, cramps, and upset stomach. Giardia can be prevented if you sterilize all drinking water while outdoors, properly clean uncooked food, (especially vegetables), and practice proper hygiene.
Lyme Disease
Bacteria: Borrelia burgdorferi
Contracted through bite of infected deer ticks. Symptoms include reddish “bulls-eye” rash around the bite, nausea, dizziness, fatigue, memory loss, heart disease, temporary or chronic arthritis. Can be prevented if you dress to minimize exposed flesh when traveling through heavy vegetation. Apply tick repellent to clothing. Check for and remove ticks found on your body after outdoor excursions. Transmission of the bacteria usually occurs late in the process of a tick bite, if you check and remove ticks prior to 24hrs of attachment, the chances of infection are very low.
Lyme disease does not typically cause symptoms in wildlife and humans cannot contract Lyme disease from properly handled meat or animal products.
More information regarding Lyme disease can be found here.
Rabies
Virus: Rabies
Contracted through contact with saliva of infected animals through bites, scratches, or mucous membranes such as the eyes, mouth, and nose. Symptoms in people include fever, headache, confusion, agitation, and eventual fatal infection of brain and spinal cord. There can also be a distinct prickling/burning sensation at the site of the bite or scratch that slowly spreads towards the head. This infection is usually fatal once first symptoms appear.
Rabies can be prevented if you avoid contact with wild animals acting sick or strange. Rabid animals can be agitated and jump or bite at imaginary objects or stimuli, have no fear of humans or be especially tame suddenly, act non-reactive and staring, pace in circles or wobble, drool excessively, or bite themselves. If you see any of these signs in wildlife, contact your local regional services office and do not approach the animal. Any mammal can become infected with rabies, but the most common carrier species that live in Newfoundland and Labrador include foxes, coyotes, dogs, and bats.
Keep pet vaccinations up to date. See your physician immediately if bitten or scratched by any animal. Do not handle the carcass of any animal suspicious of having rabies.
Trichinosis
Parasite: Trichinella
Contracted through eating raw or undercooked pork and wild game products, particularly bear, wild boar, and seals infected with Trichinella roundworms. The infective larvae are not visible to the naked eye. Symptoms include nausea, diarrhea, vomiting, fatigue, fever, and muscle pains. Death is possible in severe cases. Can be prevented if you cook meat products well. Curing (salting), drying, smoking, freezing, or microwaving meat does not consistently kill infective trichinella larvae. Clean meat grinders and utensils thoroughly if you process your own meat. Avoid infecting pets by feeding them raw meat.
Echinococcus
Parasite: Echinococcus
Contracted through contact with contaminated feces (primarily canids like dogs or coyotes) or eating raw or undercooked wild game products infected with Echinococcus eggs. Common symptoms include nausea, diarrhea, vomiting, fatigue, fever, muscle pains, while death is possible in severe cases. Can be prevented by cooking meat products well, washing your hands after handling dogs and before handling food, and cleaning meat grinders and utensils thoroughly if you process your own meat. Avoid feeding pets raw meat or organs as this may cause infection. and deworm dogs regularly, especially outdoor/hunting dogs.
The larval phase of the Echinococcus life cycle can be found as cysts in the lungs, liver, and other organs of herbivores like moose, caribou, deer, and bison. These larval cysts do not infect people but can infect dogs and scavengers. Do not eat any tissue or organ containing parasite cysts.
Intestinal Parasites in Newfoundland and Labrador
A recent study of Trichinella and Echinococcus in coyotes harvested in Newfoundland, by the University of Saskatchewan, can be found here. Below are general precautions for hunters, trappers and the general public.
- Avoid contact with fecal material when handling and skinning coyote carcasses, traps and contaminated soil.
- Choose reliable sources of drinking water
- Avoid feeding uncooked meat or organs from harvested big game to dogs
- Consult a vet about regular deworming of dogs
- Wash hands after handling pets and before handling food. Wash fruits and vegetables, including berries, with clean water before eating
- Always cook game meats to appropriate internal temperatures (at least 74 degrees C) before consuming.
- Curing (salting), drying, smoking or microwaving meats alone does not consistently kill Trichinella
- Freezing wild game meats may not effectively kill all worms because some worm species that infect wild game are freeze-resistant (ex. Trichinella).
- Clean meat grinders thoroughly after each use.
Tularemia
Bacteria: Francisella tularensis
Most commonly contracted through handling infected animal carcasses, especially rodents (muskrat, beaver, mink), rabbits, and hares. However, also possible from the bites of infected ticks and deerflies, by consuming contaminated food and water, and from inhaling aerosolized bacteria while mowing or brushing lawns heavily contaminated by infected rabbits/hare.
Symptoms in people include skin ulcers, swollen lymph glands, inflamed eyes, sore throat, and pneumonia. Most infections can be treated with antibiotics, but in severe cases the infection can be lethal. Tularemia can be prevented if you wear gloves and a mask when cleaning or handling animal carcasses, especially hares, wear appropriate long sleeve clothing and insect repellents, wear masks and goggles when mowing in rabbit/hare habitat, and thoroughly cook wild game prior to consuming. Practice proper hygiene.
The symptoms of Tularemia in animals include fever, diarrhea, vomiting, discharge from the eyes and nose, ulcers of the mouth and tongue, abscesses, starvation, and death. Do not eat animals you suspect of having Tularemia and contact your local regional services office if you see these symptoms in rodents, especially rabbits/hares.
West Nile Virus
Virus: West Nile Virus
Contracted through mosquito bites. Also direct contact with the blood of infected animals. Symptoms include fever, headache, body aches. May develop into lethal encephalitis, or swelling of the brain. Can be prevented if you wear gloves when cleaning game and cook all meat thoroughly. Reduce mosquito bites by wearing protective clothing and using insect repellents.
More information regarding West Nile Disease can be found here.
Wildlife Diseases: Important Considerations for Human Health and Food Safety
A study summary for foxes and lynx harvested in Nunatsiavut and Western and Central Labrador by the University of Saskatchewan, can be found here.
More information about health risks for hunters and trappers can be found here.









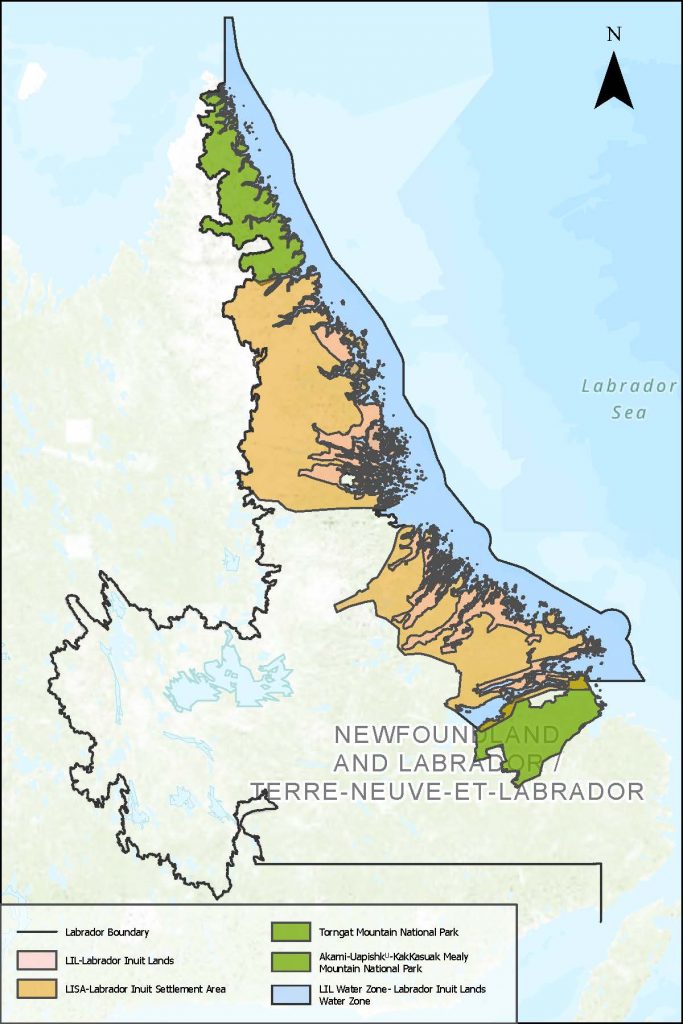


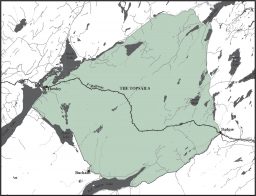


 Akami-Uapishkᵁ-KakKasuak-Mealy Mountains National Park Reserve
Akami-Uapishkᵁ-KakKasuak-Mealy Mountains National Park Reserve 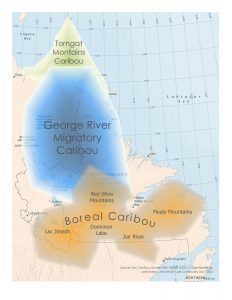
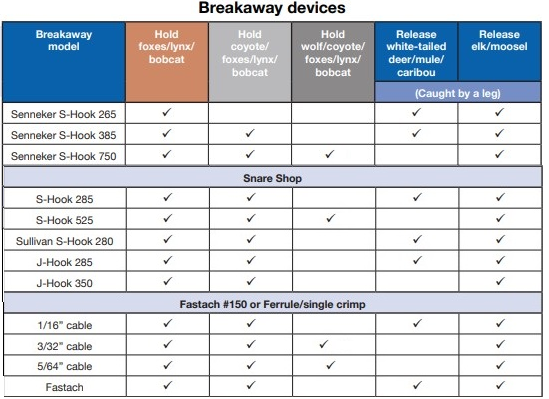
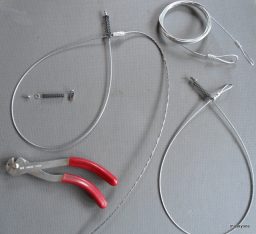 Break-away devices such as “S” or “J” hooks placed on fox, coyote, lynx or wolf snares is an easy adaptation that trappers who build their own snares can use to potentially reduce capture of wildlife such as moose, caribou and black bears or free ranging livestock. This is achieved by adding a “J” hook to the base of a slide-lock or “S” hook to a cam type lock or by adding a breakaway release ferrule (BAW) to the end of snare. The S, J hook or BAW ferrule retains enough strength to capture the intended animal but the strength of larger animals will break the hook or breakaway ferrule and allow them to escape relatively unharmed. Purchasing snares constructed in this fashion from trapping suppliers is widely available. Adding a stop to the snare so that it is still effective for capturing furbearers but allows a moose or caribou’s leg to slip through is also beneficial. There is some variability in the cost and effectiveness of break-away devices that trappers will need to consider, particularly for larger furbearers such as wolves. The end result, however, is that these devices can make a difference towards protecting wildlife or livestock that are not meant to be captured in the first place. Learn more about their use by contacting trapping supply retailers, the Newfoundland and Labrador Trappers Association or the Wildlife Division.
Break-away devices such as “S” or “J” hooks placed on fox, coyote, lynx or wolf snares is an easy adaptation that trappers who build their own snares can use to potentially reduce capture of wildlife such as moose, caribou and black bears or free ranging livestock. This is achieved by adding a “J” hook to the base of a slide-lock or “S” hook to a cam type lock or by adding a breakaway release ferrule (BAW) to the end of snare. The S, J hook or BAW ferrule retains enough strength to capture the intended animal but the strength of larger animals will break the hook or breakaway ferrule and allow them to escape relatively unharmed. Purchasing snares constructed in this fashion from trapping suppliers is widely available. Adding a stop to the snare so that it is still effective for capturing furbearers but allows a moose or caribou’s leg to slip through is also beneficial. There is some variability in the cost and effectiveness of break-away devices that trappers will need to consider, particularly for larger furbearers such as wolves. The end result, however, is that these devices can make a difference towards protecting wildlife or livestock that are not meant to be captured in the first place. Learn more about their use by contacting trapping supply retailers, the Newfoundland and Labrador Trappers Association or the Wildlife Division.